Stroke can happen suddenly to anyone, anywhere. You might be having a conversation with a loved one and notice them suddenly speaking unclearly. Or, while shopping at the grocery store, you realize you can’t move your hand to pick up a can from the shelf. Within seconds to minutes, you can go from feeling perfectly normal to feeling unwell.
Table of Contents
ToggleWhat is a stroke?
A stroke can be categorized into two main types. An ischemic stroke happens when a part of the brain is deprived of oxygen and nutrients due to a blockage or reduction in blood supply. Brain cells begin to die within minutes in this situation. On the other hand, a hemorrhagic stroke occurs when a blood vessel in the brain ruptures, causing bleeding that increases pressure on brain cells and damages them.
Signs and Symptoms
It’s important to recognize the signs of a stroke and act quickly. Knowing the symptoms can make a crucial difference:
● Facial Drooping: Check for uneven smiles.
● Arm Weakness: See if one arm drifts down when both are raised.
● Speech Difficulty: Listen for slurred speech.
● Time to Call 911: Stroke requires immediate attention. Call 911 right away and note when symptoms began.
Other symptoms include numbness on one side of the face, arm, or leg, sudden confusion or trouble understanding speech, a sudden severe headache without a known cause, sudden vision problems, and difficulty walking or maintaining balance.
If you or someone you’re with experiences any of these symptoms, seek medical help immediately.
Risk factors
Several factors can increase the risk of stroke, which can be broadly categorized as treatable and non-modifiable risk factors:
Treatable Risk Factors:
● Lifestyle: Being overweight or obese, physical inactivity, heavy or binge drinking, and use of illegal drugs like cocaine and methamphetamine.
● Medical: High blood pressure, smoking or exposure to secondhand smoke, high cholesterol, diabetes, obstructive sleep apnea, cardiovascular diseases (e.g., heart failure, heart defects, atrial fibrillation), and a personal or family history of stroke, heart attack, or transient ischemic attack (TIA).
Non-Modifiable Risk Factors:
● Age: Individuals aged 55 and older are at higher risk compared to younger individuals.
● Race/Ethnicity: African American and Hispanic populations have a higher risk compared to other racial or ethnic groups.
● Sex: Men generally have a higher risk of stroke compared to women, although women who have strokes tend to be older and face higher mortality rates.
● Hormones: Taking birth control pills or hormone therapies containing estrogen can increase stroke risk.
Additionally, factors such as COVID-19 infection have also been associated with an increased risk of stroke. These diverse factors collectively contribute to an individual’s susceptibility to stroke.
Complications
Complications following a stroke can lead to temporary or permanent disabilities, depending on the duration and location of reduced blood flow to the brain. These complications may include:
- Muscle Movement: Loss of muscle control, resulting in paralysis on one side of the body or difficulty controlling facial muscles or one arm.
- Speech and Swallowing: Impaired muscle function in the mouth and throat, causing difficulties in speaking clearly, swallowing, or eating. Language comprehension and communication skills may also be affected.
- Cognitive Function: Memory loss, difficulties with reasoning, judgment, and understanding concepts.
- Emotional Impact: Increased challenges in managing emotions and a higher risk of developing depression.
- Pain and Sensation: Pain, numbness, or tingling sensations in affected body parts, such as the arm or leg that lost feeling.
- Behavioral Changes: Potential withdrawal from social activities and increased dependency on others for daily tasks like grooming and household chores.
How is a stroke diagnosed?
Diagnosing a stroke involves several tests and procedures:
- Health History and Physical Exam: Your healthcare provider will review your medical history and conduct a physical examination.
- Brain Imaging: Tests such as CT scan and MRI provide detailed images to detect bleeding or brain tissue damage caused by a stroke. CT angiography (CTA) and magnetic resonance angiography (MRA) may also be used to visualize blood vessels in the brain.
- Carotid Ultrasound: Doppler sonography uses sound waves to assess the condition of carotid arteries, detecting any narrowing or blockages due to plaque buildup.
- Heart Tests: Electrocardiogram (ECG) records heart activity to identify irregular rhythms that could contribute to stroke. Echocardiography uses sound waves to examine the heart’s structure, size, and function, including checking for blood clots within the heart.
These tests collectively help in diagnosing stroke and identifying underlying conditions that may have led to it.
Rehabilitation
What is stroke rehabilitation?
Stroke rehabilitation, often referred to as “rehab,” aims to support individuals in reclaiming their independence and enhancing their overall quality of life. Through rehabilitation, individuals receive comprehensive assistance not only physically but also emotionally, socially, and spiritually following a stroke. The goal is to facilitate optimal health, functionality, and overall well-being. The term “rehabilitate” originates from the Latin word “habilitas,” meaning “to enable or make capable again.”
The stroke rehab team
The stroke rehab team revolves around the patient and family. The team helps set short- and long-term treatment goals for recovery and is made up of many skilled professionals, including:
- Dietitians and nutritionists
- Nursing professionals
- Occupational therapists
- Physiotherapists
- Psychologists
- Social work and counselling professionals
- Specialist medical practitioners/PRM physicians
- Speech and language therapists/pathologists
Stroke rehabilitation aids in recovering from stroke effects, relearning skills, and discovering new methods to perform tasks. The specific rehab goals and their scope are influenced by several factors, such as:
- The cause, location, and severity of the stroke
- The nature and extent of impairments and disabilities resulting from the stroke
- The patient’s overall health condition
- The level of family and community support available.
Timeline of Stroke Recovery
The correlation between timing and recovery is indisputable; initiating the recovery process sooner enhances the likelihood of regaining lost abilities.
Day 1: Initial Treatment
Upon experiencing a stroke, immediate admission to an emergency department is typically necessary to stabilize your condition and ascertain the stroke type. If the stroke is caused by a blood clot (ischemic stroke), prompt administration of clot-busting medication can mitigate long-term effects. Depending on the severity of the stroke, intensive care or acute care may be required.
Day 5-7: Continuing Care and Rehabilitation Planning
During this period, the stroke care team assesses the impact of the stroke to develop a tailored rehabilitation plan.
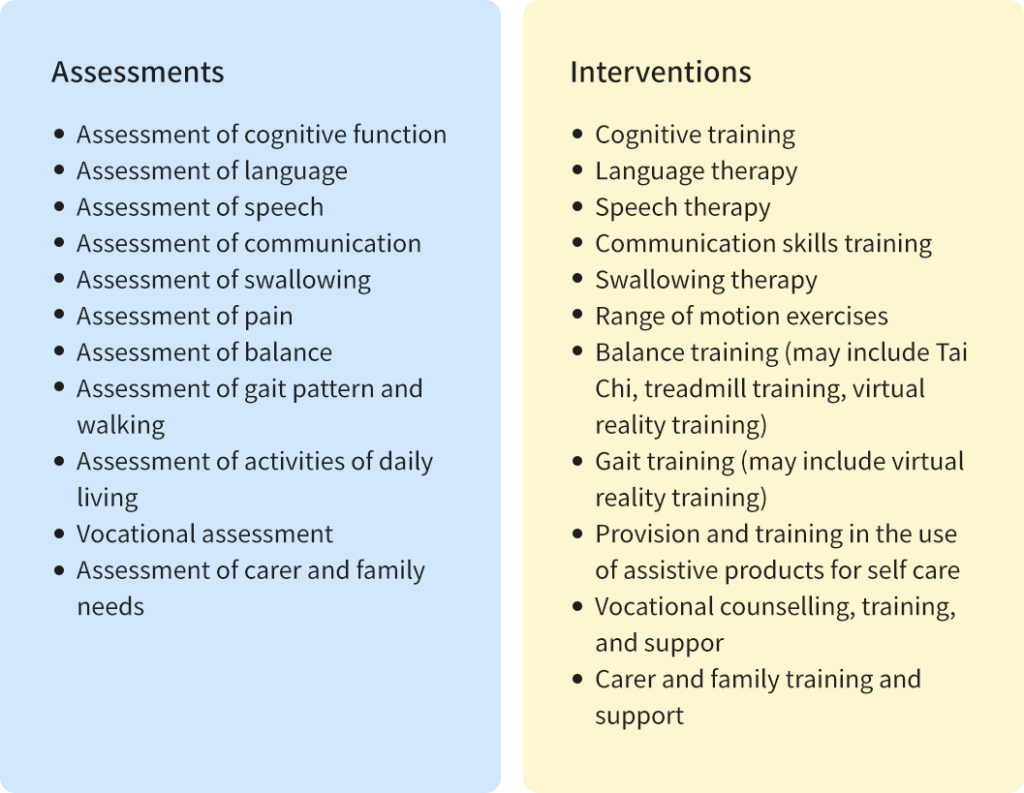
The assessments and Interventions of stroke may include the following content.
1–3 Months Post-Stroke
During this period, many patients will either participate in and complete an inpatient rehabilitation program or make advancements during outpatient therapy sessions.
The objective of rehabilitation is to restore functionality as closely as possible to levels before the stroke occurred, or to develop strategies that compensate for any functional impairments.
Post-Stroke Care Options
There are typically two main routes for post-stroke care:
Outpatient Rehabilitation:
After leaving the hospital, individuals attend therapy sessions at a rehabilitation center several times per week while residing at home.
Inpatient Rehabilitation Center:
Patients are transferred to specialized rehabilitation units or community hospitals where they receive daily therapy sessions and ongoing medical and nursing attention during their inpatient stay.
Prevention
To reduce your risk of stroke, consider the following measures:
Lifestyle Changes:
● Quit Smoking: If you smoke, quitting can significantly lower your stroke risk.
● Healthy Diet: Eat plenty of fruits, vegetables, and whole grains. Limit saturated fats, trans fats, cholesterol, sodium, and added sugars.
● Maintain a Healthy Weight: Aim for a healthy body weight through balanced diet and regular physical activity.
● Regular Exercise: Engage in physical activity most days of the week to improve cardiovascular health.
● Limit Alcohol: Drink alcohol in moderation, if at all.
Medications:
● Follow Prescribed Medications: Take medications as directed by your healthcare provider to manage stroke risk factors.
● Blood Thinners: Anticoagulants and antiplatelet medications like aspirin help prevent blood clots.
● Blood Pressure Control: Take medications to manage high blood pressure.
● Cholesterol Management: Use cholesterol-lowering drugs to reduce plaque buildup in arteries.
● Diabetes Management: Monitor and manage blood sugar levels effectively with diabetes medications.
Adopting these lifestyle changes and adhering to prescribed medications can significantly lower your risk of stroke.
Finding Community Support for Stroke Recovery
Community resources and support organizations are vital for stroke recovery. Start by contacting your healthcare provider or local hospital for recommendations on specialized stroke rehabilitation centers or outpatient clinics in your area. Online directories and national stroke associations also offer databases of local support groups. These groups provide emotional support and opportunities to learn from others facing similar challenges. Participating in community activities and joining rehabilitation groups can significantly enhance recovery by fostering motivation and a sense of belonging.
In summary, recognizing stroke symptoms and understanding rehabilitation options are vital for recovery. Make use of community resources, support groups, and medical guidance to enhance your journey. Stay proactive, communicate with healthcare providers, and seek support from loved ones. Remember, with the right resources and a supportive network, you can achieve significant improvements in your quality of life after a stroke.